Unmet Medical/Market Requirements
Currently, acute stroke is the third of the top ten causes of death in Taiwan. According to statistics of Ministry of Health and Welfare, 48 out of 100,000 people died from cerebrovascular diseases in 2015. Stroke is mainly due to vascular thrombosis, sclerosis or blocking that occurs in different parts of the brain, resulting in losses of nerve functions with varying degrees, such as sudden limb hemiplegia, aphasia or numbness of hands and feet. The current treatment methods are
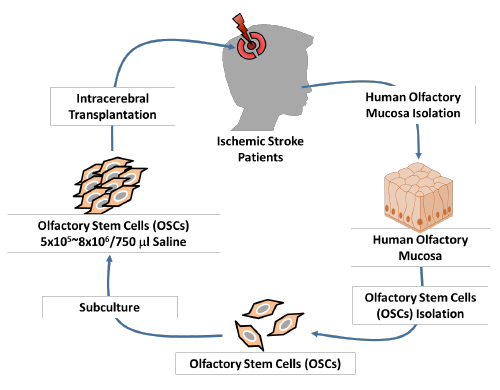
(I) Antiplatelet therapy and (II) Thrombolytic therapy. However, the former must be provided within 48 hours in the initial stage of ischemic stroke, and attention must be paid to whether patients have a history of upper gastrointestinal ulcer or bleeding. The latter is to be provided within 3 hours since the occurrence of ischemic stroke; attention must be paid to whether it results in cerebral hemorrhage or hemorrhage in the other parts of the body, and whether it is threatening to the life of patients. Therefore, currently there is only the initial first-aid treatment strategy, but no effective way for treatment of ischemic stroke. Stroke causes ischemic death in brain neural cells, and neural cells are unable to regenerate after their death. Therefore, U-NEURON BIOMEDICAL has put forward an effective treatment strategy by autologous olfactory stem cells (OSCs) to repair brain neural cells damaged by ischemia and to improve the nerve function loss and the quality of life of stroke patients.質。